Ultrasound therapy has been used for decades by both PT and OT. It’s a skilled intervention that requires training, and when used right it can be beneficial for hand therapy.
However in some circumstances, ultrasound is not effective and can be a poor use of time.
In this article, I’ll discuss when US is beneficial, ineffective, and why therapists still use it when it’s not effective.

What is ultrasound therapy?
US has been used in physical and occupational therapy to promote healing, decrease pain, reduce swelling, remodel scar tissue, and decrease inflammation.
Unlike traditional methods, therapeutic Ultrasound uses acoustic energy with modified frequencies to restore and heal soft tissues.
How does ultrasound work?

Ultrasound works by converting energy to ultrasound energy (sound waves) with an alternating current that causes vibration. These sound waves cause the molecules in a small area of tissue to vibrate and heat tissue.
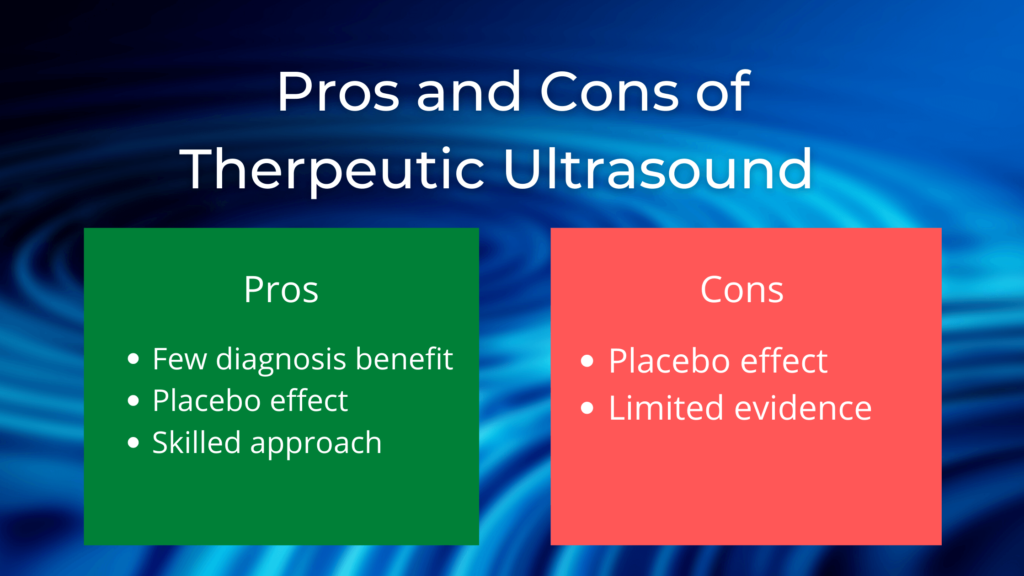
Pros and Cons of therapeutic Ultrasound
Is ultrasound effective for Hand Therapy?
According to the Physical Therapy and Rehabilitation Journal,
“There was little evidence that active therapeutic ultrasound is more effective than placebo ultrasound for treating people with pain or a range of musculoskeletal injuries or for promoting soft tissue healing”
Current studies provide little evidence to support ultrasound, but there is evidence suggesting that the more ultrasound energy that is delivered, the better the outcomes.
For instance, current treatment times of 3-5 minutes with 20-50% duty cycles, with small transducer heads might not be sufficient to provide any beneficial results.
Higher intensity US, for longer treatment periods (10-15 minutes) have been shown to provide better results.
The research also shows that ultrasound treatment is consistently effective for calcific tendinitis, scar remodeling, and carpal tunnel syndrome.
What diagnosis or injuries benefit from ultrasound?
Most of the evidence today for US in hand therapy have mixed outcomes, but much of the research has shown that US is most beneficial for treating carpal tunnel, tendonitis, and scar remodeling.
It some studies, US has been shown to reduce inflammation in tendonitis (Medial/lateral epicondylitis) and carpal tunnel syndrome.
US is also been used for scar remodeling, but is still unclear if this type of treatment is effective. For example, it can be used to reduce scar formation after surgery and increase extensibility.
This may include patients who have undergone flexor tendon repairs and have limited active range of motion.
Why PT and OT continue to use ultrasound even when it’s not effective
Working as a hand therapist, I’ve noticed that US is often overused by therapists even when it has been shown to be an ineffective treatment.
Studies have shown that the benefits of US are limited, but it’s continual use includes patients with any type of contracture, surgical procedure, or superficial scarring.
When therapists spend a large portion of treatment time using US, they often waste their time, their patient’s time, and bill charges that are not medically necessary.
In my experience, therapists use US, because it appears to be a skilled intervention. This is referred to as the placebo effect.
If therapy provides ultrasound treatment, patients will feel that they are receiving a skilled and technical intervention that isn’t replicable at home. As they continue to heal, they may feel the placebo effect in their recovery.
Is the US placebo effect bad if it encourages patients to come to therapy?
It really depends on who you are. For me, I would rather spend time working on goals that will benefit the patient in the long term.
Contraindications for ultrasound
- Cancer/Malignancy
- Hypertension
- Implants
- Pregnancy
- Active infection
- Open wound
Conclusion
According to these studies, the benefits of ultrasound continue to favor injuries related to inflammation, carpal tunnel and possibly scar remodeling.
As always, we need to be aware that as hand therapists, we treat people, not pathologies and we should keep individual factors, patient response, and patient preference in mind when selecting modalities for our clients.
References
Bakhtiary & Rashidy-Pour (2004). Ultrasound and laser therapy in the treatment of carpal tunnel syndrome
Alexander, L. D., Gilman, D. R. D., Brown, D. R., Brown, J. L., & Houghton, P. E. (2010). Exposure to low amounts of ultrasound energy does not improve soft tissue shoulder pathology: A systematic review. Physical Therapy, 90, 14-25. doi: 10.2522/ptj.20080272.
Gursel, Y. K., Ulus, Y., Bilgic, A., Dincer, G., & van der Heijden, G. (2004). Adding ultrasound to the management of soft tissue disorders of the shoulder: a randomized placebo-controlled trail. Physical Therapy, 84, 336-343.
Nimgade, A., Sullivan, M., & Goldman, R. (2005). Physiotherapy, steroid injections, or rest for lateral epicondylosis? What the evidence suggests. Pain Practice, 5(3), 203-215.
Piravej, K. & Boonhong J. (2004). Effect of ultrasound thermotherapy in mild to moderate carpal tunnel syndrome. Journal of the Medical Association of Thailand, 87(Suppl 2), S100 –S106.
Rahman, M. H., Khan, S. Z., & Ramiz, M. S. (2007). Effect of therapeutic ultrasound on calcific supraspinatus tendinitis. Mymensingh Medical Journal, 5, 33–35.
Hartzell, T.L., Rubinstein, R., Herman, M. (2012). Therapeutic modalities–an updated review for the hand surgeon. Journal of Hand Surgery, 37(3), 597-621.
As an Amazon Affiliate I earn commission from links in this post.
David is the lead editor of OT Focus. He has been practicing as an Occupational Therapist since 2013. He specializes in acute care, hand therapy, and ergonomics.



![How to reduce hand swelling [Hand Therapy basics]](https://otfocus.com/wp-content/uploads/2021/03/How-to-reduce-hand-swelling-1024x576.jpg)